Safe catheter removal and monitoring at home, helping patients regain normal bladder control comfortably.

Personalised nurse-led training to help you learn safe, effective, and independent bladder emptying techniques.
Professional guidance to maintain urethral health after surgery, preventing narrowing and ensuring smooth urination.
Regular, hygienic catheter replacement performed safely at home, reducing infection risk and maintaining comfort.

Expert management of abdominal catheters with full aseptic technique, ensuring safety, comfort, and proper drainage.
Comprehensive support for catheter hygiene, bag changes, troubleshooting, and infection prevention by skilled nurses.

Non-invasive bladder volume assessment to check urine retention and ensure optimal post-catheterisation bladder function.
For your comfort and peace of mind, all appointments are confirmed in advance, and payments are processed securely before your session.
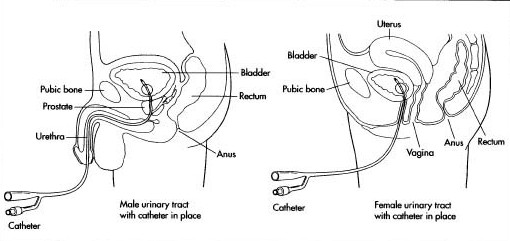
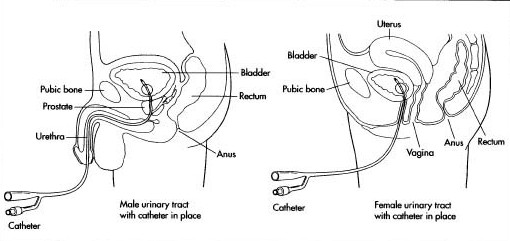
A catheter is a small tube inserted into your bladder to drain urine.
This procedure involves safely removing the catheter and assessing whether you can pass urine naturally without assistance.
Please prepare for your TWOC appointment by following these important steps:
Present a letter from your Doctor confirming that your catheter should be removed.
Stay well hydrated by drinking plenty of fluids, as you’ll need to urinate 2–3 times after removal.
Ensure you are not constipated, as this can prevent proper bladder emptying.
The nurse will remove your catheter and observe how well you pass urine naturally.
You will be asked to drink fluids and urinate two to three times.
Each time you urinate, measure and record your urine volume.
After you have passed urine two or three times, the nurse will use a bladder scanner to check if your bladder is emptying adequately.
The nurse may not stay inside your home during the waiting period but will remain nearby.
If you have passed urine twice and the nurse hasn’t returned, or if you experience difficulty passing urine, please call 0800 852 7477 for assistance.
If your bladder is emptying well, no further catheterisation will be required (Successful TWOC).
If you are unable to empty your bladder properly, you may be:
Taught clean intermittent self-catheterisation (CISC) — if suitable and you prefer not to have a permanent catheter.
Re-catheterised with an indwelling catheter — if self-catheterisation is not possible.
A detailed report will be sent to your GP and the referring professional. You’ll also receive a copy for your records.
If you develop difficulty passing urine a few hours or days after a successful TWOC, please visit your nearest Accident & Emergency department for re-catheterisation.
Pain or discomfort during catheter removal
Inability to pass urine after removal
Urinary retention occurring hours or days later
Mild bleeding during removal or reinsertion
Urinary tract infection (UTI), which can occur with any catheter procedure
Try a Trial Without Catheter today – the benefits outweigh the risks, and we’ll fully support you!
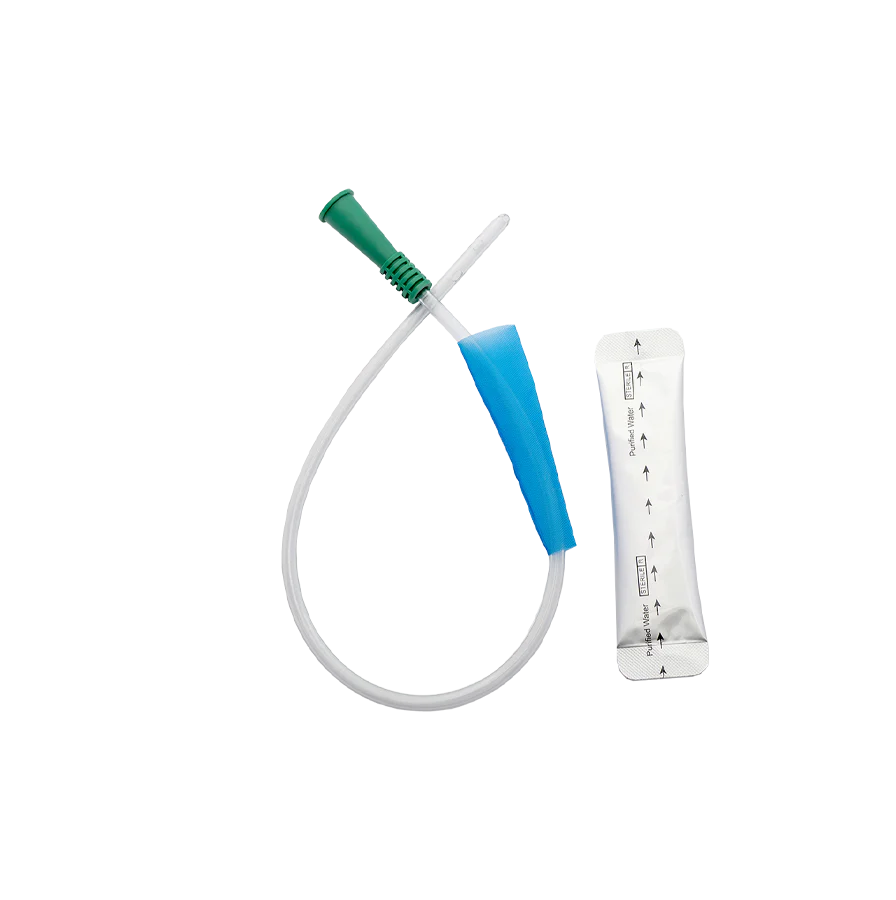
Clean Intermittent Self-Catheterisation (CISC) is a procedure in which a small catheter is gently inserted into the bladder to drain urine. The catheter is then removed immediately after the bladder has been emptied.
You will be advised how often to perform this procedure based on your residual urine volume — the amount of urine left in your bladder after you pass urine naturally.
Please ensure you meet the following requirements before your CISC session:
Present a letter from your Doctor confirming you are to be taught how to perform this procedure.
Alternatively, you may be eligible if you have failed a Trial Without Catheter (TWOC) and prefer intermittent self-catheterisation instead of an indwelling catheter.
You must be registered with an NHS GP, who can prescribe your future self-catheterisation supplies.
If you do not have an NHS GP, you may need to purchase your own catheters for future use.
A qualified nurse will guide you step-by-step through the process of safe and hygienic catheterisation.
You will be provided with a variety of clean intermittent catheters to choose from free of charge during your session.
The nurse will ensure you understand proper technique, hygiene, and storage for your catheters.
Our team will follow up via telephone after 1–2 weeks to review your progress and address any challenges you may face.
Continuous support is available to help you gain confidence and independence in performing CISC safely.
Bleeding during or after catheterisation
Pain or discomfort during insertion
Urinary tract infection (UTI) risk due to improper technique or hygiene
Difficulty or failed catheterisation caused by obstruction in the urethra
Start Clean Intermittent Self-Catheterisation confidently – we’ll support you every step!
Clean Intermittent Self-Dilatation (CISD) is a procedure that involves gently inserting a urethral catheter or dilator into the urethra and removing it shortly after. This helps to keep the urethra open (patent) — usually following a surgical procedure performed to widen a narrowed urethra.
To ensure safety and correct timing for your CISD training:
Please provide a letter from your Urologist or GP confirming that you require self-dilatation training.
The letter should also specify how many days after your surgery the session should take place.
A trained nurse will guide you step-by-step through the self-dilatation technique, ensuring comfort and confidence.
You will be shown how to perform the procedure safely and hygienically, using the correct equipment.
The session will include advice on frequency, cleaning, and lubrication to maintain urethral health.
Bleeding during or after insertion
Pain or discomfort during dilatation
Urinary tract infection (UTI) caused by improper hygiene
Difficulty or failed catheterisation/dilatation due to urethral obstruction
Book your Clean Intermittent Self-Dilatation session – safe, effective, and fully supported!
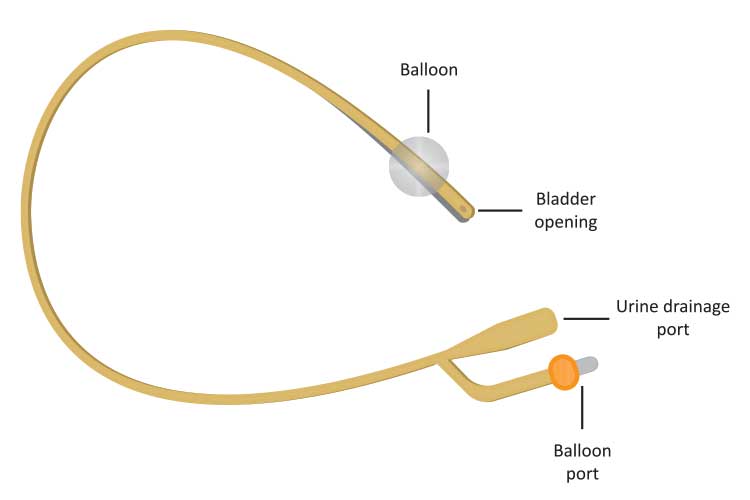
This procedure is designed for patients with a long-term urethral catheter that requires regular replacement — typically every three months.
A catheter is a thin, flexible tube aseptically inserted through the urethra to drain urine from the bladder. Regular changes help prevent blockages, infections, and maintain comfort.
To ensure a safe and efficient catheter change, please:
Provide documentation of your last catheter change so we can confirm when you are due for your next one.
Note that some catheters may need to be changed earlier due to blockages or other complications.
Ensure you have your catheter and Instillagel available at home before your appointment. (Your GP may prescribe these for you.)
You may also purchase your own catheter pack or tray before your appointment, or we can provide them at an additional cost — please refer to our brochure for details.
The nurse will perform the catheter change using aseptic technique to maintain hygiene and prevent infection.
The process is quick and performed with care to ensure minimal discomfort.
After the procedure, your nurse will confirm proper urine flow and catheter placement.
Pain or discomfort during removal or insertion
Bleeding or trauma to the urethra
Difficulty or failure to reinsert the catheter
Urinary tract infection (UTI) following the procedure
A suprapubic catheter is a urinary catheter that is aseptically inserted into the bladder through the abdomen, rather than the urethra. This procedure is usually performed for patients who require long-term bladder drainage or have difficulty with urethral catheterisation.
To prepare for your suprapubic catheter change, please:
Provide documentation of your last catheter change so we can confirm if you are due for a replacement.
Be aware that a catheter may need to be changed earlier than scheduled due to blockage or other clinical reasons.
Ensure you have your catheter and Instillagel available at home before your appointment. (Your GP may prescribe these for you.)
You may also purchase your own catheter pack or tray, or request ours at an additional cost — please refer to our brochure for pricing details.
We recommend keeping the catheter insertion site open (without a dressing) if it is not weeping, as this allows the area to dry faster and heal properly.
The nurse will carefully remove the existing catheter and insert a new one using aseptic technique to prevent infection.
The procedure is typically quick and performed with gentle care to ensure patient comfort.
The nurse will confirm proper catheter placement and drainage before completing the visit.
Pain or discomfort during or after insertion
Bleeding at the insertion site
Difficulty or failure to reinsert the catheter
Urinary tract infection (UTI)
Our Catheter Care service focuses on maintaining the cleanliness, function, and comfort of your urinary catheter system. Proper care helps to prevent infections, blockages, and discomfort, ensuring your catheter works efficiently and safely at all times.
This service includes:
Cleaning the catheter insertion site to reduce infection risk.
Changing urinary drainage bags and flip-flow valves for hygiene and comfort.
Performing catheter flushes or bladder washes to maintain a clear flow and prevent blockage.
Please ensure you have your catheter flushes ready on the day of your appointment.
If you require regular catheter flushes due to debris or frequent blockages, your GP can prescribe the necessary supplies.
Helps maintain a clean and functional catheter system.
Prevents infection and blockages caused by debris or bacteria.
Ensures patient comfort and confidence through professional nursing support.
Bladder scanning is a non-invasive ultrasound test that measures the amount of urine left in the bladder after you pass urine (post-void residual). It helps assess how well the bladder is emptying and guides further care decisions.
Symptoms of incomplete emptying (urgency, weak stream, dribbling).
After catheter removal to check bladder function.
For monitoring patients with bladder dysfunction or long-term catheters.
During a trial without catheter (TWOC) to prevent bladder over-distension.
A trained nurse places a small probe over your lower abdomen using ultrasound gel.
You may be asked to void first, then be scanned to measure remaining urine.
The scan is quick, painless, and avoids invasive catheter measures when possible.
Results inform whether monitoring, further intervention, or no action is needed.
Reduces unnecessary catheterisations and their risks.
Provides clear, objective measurements to guide your care.
Offers reassurance and helps plan appropriate next steps.
High residual volumes may indicate retention and require further assessment.
Certain factors (for example, obesity or prior abdominal surgery) can affect scan accuracy.